4chan
Adolescent
Adult
AFAB (FAAB)
Affirmative care
AGAB
Agender
Ally
Alphabet mafia
Altersex
American Civil Liberties Union (ACLU)
Androgyny
Anti-defamation League (ADL)
Asexual (ace)
Autogynephilia (AGP)
anatomical, focusing on having a woman’s body or body parts;
physiological, focusing on bodily functions that only females have;
behavioural, focusing on activities seen as feminine; and
transvestic, focusing on wearing women’s clothes.
Autoandrophilia (AAP)
AMAB (MAAB)
Anti-androgens
Finasteride blocks an enzyme involved in testosterone metabolism and is prescribed to treat hair loss and benign prostatic hyperplasia (enlargement of the prostate) in males. Some females may also use it, such as females who ‘transition’ to ‘male’ and experience unwanted male-pattern baldness. This kind of use can come with unwanted side effects such as redistribution of fat, reduction of sex drive, and the return of menstruation.
Authentic self (true self)
BBL (Brazilian butt lift)
BDSM
Bimboification
Binder
Binding
Binge and purge
Biological sex
Biphobia
Bisexual
Blåhaj
Blaire White
Blanchard’s typology of transsexualism
Body dysmorphic disorder (BDD)
Body integrity identity disorder (BIID)
(Boomer)hon
Born in the wrong body
Bottom growth
Bottom surgery
Boxer ceiling
Boy
Boy mode (boymoding)
Boygasm
Breast augmentation
Buck Angel
Bussy
Butch
Caitlyn Jenner
Caster Semenya
Chaser
Chastity/Chaz Bono
Chestfeeding
Christine Jorgensen
Christine Weston Chandler (Chris Chan)
Cisgender (cis)
Clavicle-shortening surgery
Clinical trial
Clocking
Coming out
Comorbidity
Concern trolling
Consistent, insistent, and persistent
ContraPoints
Conversion therapy
Cope and seethe
Cosmetic surgeon
Cotton ceiling
Crossdressing
Cross-gender identity
Cross-sex hormones
Crybully
DARVO
David Reimer
Dead name
Desistance
Detransition
Dilation
Discord
Disorder of sexual development (DSD)
DIY HRT
Donor site
Double mastectomy (bilateral mastectomy)
Double incision, creating two horizontal incisions across the upper chest
Double incision that meets in the middle to create one long incision across the upper chest
Inverted T with, for each breast, an incision around the nipple, a horizontal incision on the upper chest, and a vertical incision connecting the two
Fish mouth that leaves a higher horizontal scar on each side of the chest with a scar around the nipple and this nipple placed in the middle of the horizontal scar
Peri areolar leaving scars around the nipples
Keyhole, leaving scars around part of the nipples
Other variations
The nipples may be completely removed and replaced as a skin graft (‘free nipple grafts’) and some patients choose to have the nipples removed permanently because of anticipated benefits for healing and/or they don’t want to keep their nipples for other reasons. In some countries, these surgeries are performed on minors as young as 12 years of age. Breast tissue does not grow back, and it is possible to permanently lose sensation in the nipples or be left with unusual/unpleasant sensations in the nipples as a result of the surgery (in surgery types that retain the nipples). Because the breasts are removed, breast feeding is no longer possible.
Douching
Dox(x)ing
Drag king
Drag queen
Drag queen story hour
DSM
Echo chamber
Eddie Izzard
Egg
En femme
Endocrinologist
Equality Act 2010
Eugenics
Eunuch
Eunuch Archives
Euphoria boner
F2M
Facial feminisation surgery (FFS)
Cheek augmentation using implants, or breaking the cheekbones and placing them into a different position, or through taking fat away from one part of the body and injecting it into the cheeks.
Chin width reduction to shorten and narrow the chin by removing some of the bone.
Eye and lid modification which cuts away excess tissue.
Forehead contouring removing parts of the forehead bone to reduce frontal bossing.
Hairline lowering which removes forehead skin along the hairline.
Hair transplantation that removes hair from one part of the head to place in balding areas.
Jaw angle reduction by removing parts of the lower jaw.
Lip lift, which takes away some of the tissue between the nose and upper lip, and lip augmentation through fillers, implants, or fat injection of fat removed from elsewhere on the body.
Rhinoplasty (‘nose job’) to change the shape/size of the nose.
Tracheal shave which removes/reshapes part of the thyroid cartilage (Adam’s apple).
Faʻafafine and Fa'afatama
Facial masculinisation surgery (FMS)
Adam’s apple surgery that uses cartilage from another part of the body to create the appearance of an Adam’s apple.
Cheek surgery using implants to make the cheeks more angular.
Forehead surgery aiming to create a wider forehead.
Chin surgery using bone, implants, or fat to broaden the chin or make the jawline appear sharper.
Hair transplantation that removes hair from one part of the body to place on the face.
Nose surgery using cartilage or bone grafts to enhance the nose.
Fallon Fox
Fauxgina
Female
Since transgenderism has gained so much visibility, reductionist and dehumanising terms have started to be used to refer to females, possibly in an effort to not upset/offend TiMs and TiFs. This includes:
menstruator
people who menstruate
uterus-haver
people with a vagina
people with a cervix
birthing parent
non-man
etc.
Fair Play For Women has made a graphic showing some of the different terms used to refer to females in light of transgenderism:
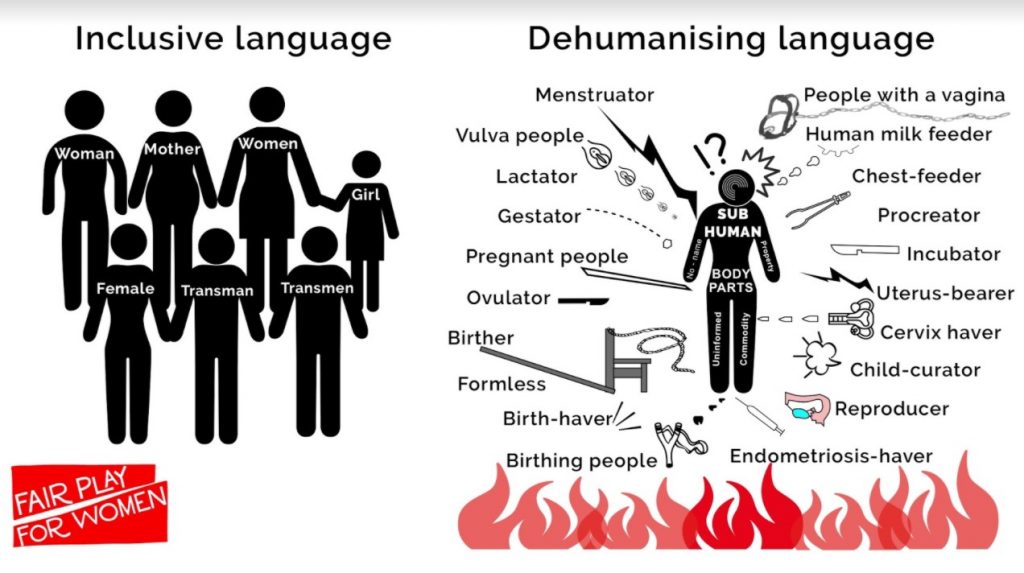
From Fair Play For Women, https://fairplayforwomen.com/language2/ .
Interestingly, this kind of language change has mostly/only been applied to females and not to males. Males are still called men or boys, not: penis-havers, people who ejaculate, people with a prostate, etc.
Female masking
Femboy
Femcel
Feminine essence
Feminism
Fetish
FetLife
Female genital mutilation (FGM)
Flag
Forced feminisation
Front hole
FtM
Furry
Futanari
Gaff
Gatekeeping
Gay
Gay-Straight Alliance (GSA)
Gender
Gender affirmation surgery (GAS)
Gender binary
Gender-based violence
Gender critical (GC)
Gender confirmation surgery (GCS)
Gender creative
Gender diverse
Gender dysphoria
Contrasts with gender euphoria. According to transmedicalists you need to experience gender dysphoria in order to be trans. According to other trans-identifying people, you don’t need to experience gender dysphoria to be trans and experiencing gender euphoria is enough to call yourself trans. Others will consider anyone who identifies as trans for any reason, as trans. Not everyone who experiences gender dysphoria will identify as trans.
Gender euphoria
Gender expansive
Gender expression
Gender fluid
Gender identity
Gender identity disorder (GID)
Gender incongruence
Gender non-conforming (GNC)
Gender reassignment
Gender recognition act (GRA) 2004
Gender recognition certificate (GRC)
This means that males who still have their penis and testicles and have typical male strength and libido can legally be recognised as female. Secondly, the language refers to ‘gender’ but what is changed with the GRC is legal sex.
Gender recognition surgery (GRS)
Gender roles
Gender Unicorn
Genderbread Person
Genderqueer
Gender variant
Genital preference
GIRES (Gender Identity Research and Education Society)
Girl
Girl dick
Girlgasm
GLAAD (Gay & Lesbian Alliance Against Defamation)
GnRH analogues/agonists
Gold-star lesbian
Grooming
Gynaecologist
Gynaecomastia
Gynandromorphophilia (GAMP)
Hair removal
Harm reduction
He-ma’am (GameStop Trans)
‘Her’
Hermaphrodite
Heterosexual
Hijra
Hipbone implants
Homophobia
Homosexual
Homosexual transsexual (HSTS)
HRC (human rights campaign)
HRT (hormone replacement therapy)
In TiMs:
titty skittles
antiboyotics
anticistamines
Fem&Ms
tit tacs
breast mints
womentos
vitamin E
the Notorious HRT
In TiFs:
T
boy juice
proboyotics
Hugboxing
Hypothalamic-pituitary-gonadal (HPG) axis
Hysterectomy (‘hysto’)
When the gonads (in this case, ovaries) are removed, the person will have to take hormones for the rest of her life because her body can no longer make enough of its own sex hormones.
I am Jazz
Incel
Incel to trancel pipeline
Indication
Informed consent
Informed consent is the process in which a health care provider educates a patient about the risks, benefits, and alternatives of a given procedure or intervention. The patient must be competent to make a voluntary decision about whether to undergo the procedure or intervention. Informed consent is both an ethical and legal obligation of medical practitioners in the US and originates from the patient's right to direct what happens to their body. Implicit in providing informed consent is an assessment of the patient's understanding, rendering an actual recommendation, and documentation of the process. The Joint Commission requires documentation of all the elements of informed consent "in a form, progress notes or elsewhere in the record." The following are the required elements for documentation of the informed consent discussion: (1) the nature of the procedure, (2) the risks and benefits and the procedure, (3) reasonable alternatives, (4) risks and benefits of alternatives, and (5) assessment of the patient's understanding of elements 1 through 4. [Shah et al., StatPearls Publishing, 2022]
However, in transgender healthcare, ‘informed consent’ is generally used to refer to a way of receiving treatment that does not have such a stringent process but in practice means that someone can visit a healthcare practitioner once or twice and then receive a prescription for drugs or support letters for surgery on the assumption that this is what the patient wants, and that the patient knows what is best for them. It appears a lot less like traditional medical practice and more like ordering a product off the internet.
Can a parent consent on behalf of their child? We all assume parents try to do the best for their child but some are harming their kids knowingly (Munchausen syndrome by proxy – 'transhausen by proxy'). Can adults not fall victim to ideology (some religious groups forbid blood transfusion for themselves including any children in their care; some religious groups perform circumcision on their children)? If the child grows up to resent this happening to them, who do they take issue with, the ideology? The MDs? The parents?
Informed consent clinic
Intersectionality
Intersex
Jazz Jennings
Jessica (Jonathan) Yaniv
J. K. Rowling
Journey
Julie Bindel
Karen White
Kathoey
Keira Bell
Kink
Kinsey scale
Kiwi Farms
Kayla Lemieux
Laurel Hubbard
Laverne Cox
Lesbian
Lesbian erasure
LGB Alliance
LGBT history month
LGBT pride month
LGBTQIA+ etc
+, who knows?
Lia Thomas
Linda Ann Bellos OBE
Lived experience
Living your best life
Love bombing
M2F
Male
Male genital mutilation (MGM)
Man
Dr Marci Lee Bowers
Maya Forstater
Meat Lego
Medical transition
Men’s Rights Activists (MRAs)
Meninism
Mermaids
Meta-analysis
Metoidioplasty (‘meta’)
There are variations to this surgery such as not having the urethra rerouted/extended or not opting for a vaginectomy. The result is a ‘micropenis’ of sorts which is likely not able to penetrate a vagina or anus. This surgery does not take a full-thickness skin graft at all so there will be no scars elsewhere on the body (unlike in phalloplasty bottom surgery).
MGTOW
Minodoxil
Minor (child)
Misgendering
Misandry
Misogyny
MLM (MSM)
MtF
Narcissistic rage
Natal sex
Neophallus
Neopronouns
Neovagina
Neurogender
NHS
Nonbinary (NB) (enby)
Non-disclosure agreement (NDA)
Non-op
Nullo
Oestrogen
- blood clots
- heart problems
- discharge from the nipples
- weight gain
- type 2 diabetes
- stroke
- infertility (but oestrogen is not a form of birth control)
- high blood pressure
- high levels of triglycerides (a kind of fat), potassium, and the hormone prolactin in the blood
- increased risk of breast cancer
Off-label use
Oli London
OnlyFans
Oppression Olympics
Some people engage in this by broadcasting all of their perceived disadvantages on their social media profiles or by bringing them up in discussions or debates. Anyone who is an ethnic minority is seen as being oppressed vs others who are of the dominant ethnicity. Anyone who has a non-straight sexuality is seen as being oppressed vs others who have a straight sexuality. A trans identity ‘trumps’ not having a special gender identity. Having a mental illness trumps not having a mental illness. Having a physical disability trumps being able bodied, etc. Having multiple ‘disadvantages’ makes you more oppressed: a gay black male is more oppressed than a gay white male; a disabled person who identifies as trans is more oppressed than a disabled person who does not identify trans, etc. This ‘game’ of supposedly being the most oppressed is won by the person highest on the totem pole of oppression. However, it is not clearly defined who this is when people with an equal number but different perceived disadvantages ‘compete’: Is a religious-minority gay black male more or less oppressed than a trans-identifying disabled white female?
Orchidectomy (orchiectomy, ‘orchie’)
Outing
Packer
Paedophilia
Pansexual
Paraphilias
Paraphilic infantilism
Passing
Peak trans
Peer-review
Penectomy
Penile-preserving vaginoplasty
PFLAG
Phalloplasty (‘phallo’)
Radial forearm free flap (RFF) phalloplasty uses tissue of one of the forearms leaving a big hole on the forearm.
Anterolateral thigh flap (ALT) phalloplasty uses tissue of one of the thighs leaving a big hole on the thigh.
Musculocutaneous latissimus dorsi flap (MLD) phalloplasty uses tissue from the back leaving a big hole on the back area.
Abdominal (‘abdo’) phalloplasty uses tissue flaps from the abdominal area that are flipped around and stitched together to close the hole created by removing this tissue.
Single-scar phalloplasty (SSP) uses a skin expander on the thigh that needs to be regularly filled to create excess skin. This extra thigh tissue is then used to create the neophallus. The patient is left with a line scar only as opposed to a big hole at the donor site.
Superficial circumflex iliac artery perforator (SCIP) flap phalloplasty uses skin and tissues in the waist area to create the neophallus, leaving a single scar.
Gracilis muscle flap phalloplasty uses the gracilis muscle (located on the inside of your upper legs) to help build the neophallus in an effort to prevent fistulas from forming. Other donor tissue may also be used.
The neourethra will be created from another full-thickness skin graft that is taken from, for instance, the forearm, or may be created from a buccal graft (the inside of the mouth), the labia minora, or the vagina. The clitoris can be buried underneath the skin at the base of the neophallus or left exposed on the outside of the body.
When using one of the techniques that leave a big hole at the donor site, this hole will need to be covered with a split-thickness skin graft from another part of the body. Such a graft only takes a thin layer of shaved skin from the donor site for this graft, leaving a relatively faint scar once healed.
Testicular implants can be inserted into the ‘neoscrotum’. Of course, these are cosmetic only as they will not create sperm.
It is possible to have some kind of erectile functionality in the neophallus by getting a penile implant. There are three types of implants:
A non-inflatable, semi-rigid implant that can be either malleable or non-malleable. This provides some rigidity to the neophallus but there is no option to go from ‘flaccid’ to ‘erect’: the neophallus will only have one rigidity state and can be bent up or down to create an ‘erection’.
A 2-piece inflatable implant.
A 3-piece inflatable implant.
The inflatable implants are composed of cylinders, a pump, a reservoir, and a control toggle. This makes it possible to alternate between a ‘flaccid’ and an ‘erect’ state. These implants are at a higher risk of malfunction and may need to be replaced several times over the course of someone’s life.
There are risks associated with a penile implant, such as erosion of the implant through the penile tissues (when parts of the implant make a hole in the skin through constant pushing onto the skin; once the skin is broken, there is a risk of infection). The cylinders may also come lose from the rest of the implant meaning a surgery is needed to try to put them back or replace the whole implant.
These surgeries are not like typical cosmetic surgeries in that they are experimental and aim to add a function that the patient never had (meaning these procedures done in females are not reconstructive (a phrase that is sometimes used): you can’t reconstruct something that was never there and never meant to be there in the first place).
For a longer description including photos of some phalloplasty procedures, see https://tau.amegroups.org/article/view/26419/24265 ('Phalloplasty: techniques and outcomes', by Aaron L. Heston et al. in Vol 8, No 3 (June 27, 2019) of Translational Andrology and Urology).
Phallus/Phallo
Planned Parenthood
Plastic surgeon
Post-op
Pre-op
Precocious puberty
Preferred pronouns
Progesterone
Pronouns
Puberty blockers
Queer
Queer theory
Questioning
Randomised controlled trial
Rapid-onset gender dysphoria (ROGD)
Real-life test (real-life experience)
Red Pill
‘The Red Pill’ is an online movement by men who feel they are now awake to the (perceived) reality that as men they don’t have systemic power or privilege (these men are ‘redpilled’), as opposed to ‘blue-pilled normies’ who believe the mainstream narrative that males automatically have privilege over females. ‘The black pill’ refers to beliefs held by people in the incel community such as biological determinism, fatalism, and defeatism for unattractive people. See: https://en.wikipedia.org/wiki/Incel#%22Red_pill%22_and_%22black_pill%22
Renée Richards
ReSisters
Retransition
Reverse dysphoria
Review (literature review)
Revision
Rib removal
RuPaul
Salmacian
Self ID
Sex
‘Sex assigned at birth’
Sex-based right
‘Sex is a spectrum’
Sex reassignment surgery (SRS)
Sexual fetishism
Sex stereotypes
Sexual dimorphism
Sexual orientation/sexuality
Sharron Davies
Shenis
Dr Sidhbh Gallagher
Sissy
Sissy hypno
Sissification
Standards of Care (SOC)
Stefonknee Wolscht
Stonewall
Social media
Social transition
SSSS (quad-S)
Statistics
Stealth
STP
Subreddit (‘sub’)
Super straight
T4T
T dick
Tanner scale
Trans-exclusionary radical feminist (TERF)
Testosterone
Testosterone use in females can have the following effects and side effects:
Skin will thicken and become more oily, pores will become larger
Increased sweating
Change in odour of sweat and urine
Acne
Increase in body hair and in thickness of the hair, facial hair growth, and possibility of male-pattern baldness or complete hair loss
Redistribution of bodyfat away from thighs and hips and towards the belly; fat in your face will distribute differently, somewhat changing your facial features
Increase muscle definition and increase in muscle mass depending on exercise
Veins become more prominent
Voice will lower due to thickening of the vocal cords
Vaginal atrophy similar to post-menopausal women (dryness, irritation, bleeding during penetration)
Loss of menstrual period (but testosterone is not a form of birth control)
Weight gain
High blood pressure
Increase in cholesterol (possibly increasing risk of heart problems)
Sleep apnoea
Type 2 diabetes
Pelvic pain
Infertility (but testosterone is not a form of birth control)
(Painful) growth of the clitoris
Blood clots
Producing too many red blood cells (polycythaemia)
It is not possible to pick and choose which effects a female will experience. Some females use a relatively low dose (‘microdosing’) in an effort to prevent too much virilisation (virilisation is the process in which a female develops characteristics associated with male hormones) but that is not a guarantee for preventing a full beard or male-pattern baldness, for instance.
Testosterone can be administered in different ways. A common way is injection but there are also ‘pellets’ (a small implants placed under the skin), a patch that is stuck onto the skin, oral capsules, and gel. Use of testosterone gel can be harmful to people around the user as the gel can rub off on others (called secondary exposure; the drug can affect people of all ages, including children of any age, and can cause premature puberty and genital enlargement in children).
The FDA has only approved testosterone products “for use in men who lack or have low testosterone levels in conjunction with an associated medical condition.” The use of testosterone by females is thus experimental.
Tgirl (t-girl)
TikTok
Toe shortening surgery
Tomboy
Top surgery
Tracheal shave
Trancel
Tranny
Transbian
Transboy (trans boy)
Transbucket
Transhausen-by-proxy/Trannyhausen-by-proxy
Trans-identifying female (TiF)
Trans-identifying male (TiM)
Trans
Trans day of remembrance (TDOR)
Trans day of visibility (TDOV)
Transgender
Transgenderism/transgender ideology
Transgirl (trans girl)
Trans feminine (trans femme)
Trans masculine (trans masc)
Transmaxxing
Transition
Trans joy
Transman (trans man)
Transmedicalism (transmedicalist)
Transperbole
Transracial
Trans rights activist (TRA)
Transsexual
Transtrender
Trans widow
Transwoman (trans woman)
Trans tape
Transcel
Transphobia
Transvestic fetishism
Transvestite (TV)
Trap
Triggered
Truscum
Tucking
Tucute
Tumblr
Two-spirit (2S)
Urologist
Vaginectomy
Vaginoplasty
In penile-inversion vaginoplasty (PIV) the skin of the penis is used to create the canal.
In peritoneal pull-through (PPT) vaginoplasty, peritoneum (lining of the abdominal wall) is used to create the canal.
Tunica vaginalis (tissue that sits around the testes) can be used to create the canal.
A part of the sigmoid colon can be used to create the canal in a technique called intestinal vaginoplasty.
A less common form of this surgery is penile-preservation vaginoplasty (PPV). The penis is left alone whilst other tissues are used to create a canal in the perineum. This can include removal of the testes and using the scrotum to create ‘labia’. Alternatively, the testicles and scrotum are left intact, and the patient only has a canal in the perineum without any ‘labia’.
When someone has undergone this surgery, they will need to dilate to prevent the canal from closing up. This means that the person will need to use hard plastic/glass dildos to keep the canal from closing up in several sessions a day in the first weeks/months after surgery. The frequency of dilation can usually be reduced to a couple of times a week once the person has healed.
When the gonads (in this case, testes) are removed, the person will have to take hormones for the rest of their life because their body can no longer make enough of its own sex hormones. The patient is also infertile after the testes are removed.
This surgery creates a canal that ends in a dead end: there will not be a cervix or uterus. Uterus transplants are experimental in females and even more experimental in males. This is not something offered currently or likely ever as a uterus transplant is for the purpose of pregnancy. This would involve a foetus who did not consent to being part of a medical experiment.
These surgeries are not like typical cosmetic surgeries in that they are experimental and aim to add a function that the patient never had, meaning these procedures done in males are not reconstructive (a phrase that is sometimes used): you can’t reconstruct something that was never there and never meant to be there in the first place. This also applies to the TiF genital surgeries.
Valid
Dr Veronica Ivy/Rachel McKinnon
Virtue signalling
Vocal feminisation surgery (VFS)
Vulvoplasty (zero-depth vaginoplasty)
Watchful waiting
Wi Spa
Woke
Woman
Womanface
WPATH (World Professional Association for Transgender Health)
Wrong-sex hormones
Yaoi
Yeeting
YouTube
*** MINI MEDICAL DICTIONARY ***
You can find a lot of first-person accounts of medical transition (use of drugs and cosmetic surgeries) on YouTube, in Reddit communities, (closed) Facebook groups, and sometimes in news articles.
Blood clot
Blood can form clots during/after surgery. These can cause problems when they get stuck in an artery and prevent blood from reaching certain tissues or organs (such as in the case of a pulmonary embolism, where a blood clot blocks blood flow to a lung, or in an ischaemic stroke where a blood clot blocks bloodflow to the brain) or when they prevent blood from flowing back to the heart (such as in deep vein thrombosis). It is possible to lose a limb to a blood clot. You can have permanent brain damage from an ischaemic stroke (caused by a blood clot). It is also possible to die from a blood clot that is not treated in time.
Blood loss
Losing blood is a risk for any surgery. When too much blood is lost the patient may need to receive a blood transfusion (where blood from other people is given to the patient to replace the blood the patient lost).
Bone health
Bone development takes place throughout childhood and puberty is one of the periods of rapid bone growth and mineralisation. Sex hormones are essential for bone maturation during puberty (see https://www.frontiersin.org/articles/10.3389/fendo.2022.967711/full). Use of puberty blockers (gonadotropin-releasing hormone (GnRH) analogues (GnRHa)) or progestins to block the body's own production of sex hormones can affect bone development and increase the risk for osteoporosis later in life (see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9150228/). A review from 2022 states: "Results consistently indicate a negative impact of long-term puberty suppression on bone mineral density, especially at the lumbar spine, which is only partially restored after sex steroid administration." (see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9578106/). The NY Times dedicated an article to puberty blockers used in transgenderism and shared an anecdote about a Texas teenager who had very low bone density in the lumbar spine (the lower back) after a year on puberty blockers. No scan was performed at baseline (before the treatment) so it is possible this child had a low value to begin with, but because no scan was performed before use of the blockers, they will never know. The story of another teenager was also included. This teen took drugs from age 11 to 14 and no scans were performed until the last year of treatment. This patient developed osteoporosis and experienced a compression fracture in the spine with continued back pain as a consequence of this permanent disability caused by puberty blockers (see https://www.nytimes.com/2022/11/14/health/puberty-blockers-transgender.html).
Breast implant illness (BII)
This is a systemic complication associated with breast implants. Signs and symptoms can include joint and muscle pain, chronic fatigue, breathing problems, anxiety, depression, headaches, hairloss, memory and concentration problems. Women who have silicone gel-filled implants were more likely to be diagnosed with auto immune conditions such as Sjogren syndrome, scleroderma, or rheumatoid arthritis. Find more information here: https://www.breastcancer.org/treatment/surgery/breast-reconstruction/types/implant-reconstruction/illness/breast-implant-illness.
Catheter
A suprapubic (SP) catheter is inserted into the bladder through a hole made into the abdomen (belly); a Foley catheter is inserted through the urethra (the tube that transports urine from your bladder to the outside of your body) and held in place in the bladder by a water-filled balloon. Depending on the type of genital surgery and whether you have complications, you may only need a catheter for a few days or in extreme cases for months at a time.
Colostomy, ileostomy, urostomy
An ostomy is surgery to create an opening (stoma) from an area inside the body to the outside. This is done when there are issues with the tissue further down so the damaged area is avoided by funelling the body fluid out of the body before the problem area.
A colostomy is an opening from the colon (large intestine) to the outside through the abdomen (belly). A colostomy bag is then attached to catch the fecal matter (poop, stool). This bag needs to be emptied/replaced several times a day to every couple of days depending on the type of bag and consistency of stool. You may need a colostomy for a shorter period of time or for the rest of your life depending on what the reasons are. A temporary colostomy may be needed after colon surgery to remove cancer, for instance. You may end up with a permanent colostomy if a certain part of the colon had to be removed or permanently rested, or if you can not undergo more surgery due to other health problems. Information on living with a colostomy: https://www.nhs.uk/conditions/colostomy/living-with/.
An ileostomy is an opening from the small intestine to the outside through the abdomen (belly). This is performed when the colon needs to be removed of rested after surgery or treatment. A stoma bag is then attached to catch the fecal matter (poop, stool). This bag needs to be emptied/replaced. Information on ileostomy: https://www.nhs.uk/conditions/ileostomy/.
A urostomy is performed when someone's bladder is removed or urine can't pass through the bladder and urethra (for instance due to damage to the urethra after surgery). The procedure creates a stoma for the urinary system by using a bit of intestine. Also called an 'ileal cinduit urinary diversion'. The urine is collected in a pouch on the outside of the body.
Death
Every surgery comes with the risk of death either from the anaesthesia or the procedure itself, but usually death is a very rare surgical outcome. Certain factors may increase the risk of death from the surgery, such as in emergency operations, when the patient is of an older age, or when the patient undergoes a major procedure. See https://pubmed.ncbi.nlm.nih.gov/24021395/ for information in mortality (death) risk in various surgeries.
Death is a possible consequence of genital surgery for gender reasons, as described in a case study on an 18-year-old male who underwent vaginoplasty, who died from the results of an E. coli infection, see https://www.sciencedirect.com/science/article/abs/pii/S1083318816301747.
Dilating difficulties
Dilation is the process of using hard dildos to keep open the neovaginal canal/tunnel. This is required after vaginoplasty surgery to ensure the canal does not heal shut or shrink in length or width. It is possible to experience a lot of pain during dilation. A YouTuber ('Adea') who had vaginoplasty explained how he was in so much pain he was sweating and nearly passed out from dilation. Other people may experience less pain or even no pain but this might be due to nerve damage. This could result in them being rougher with their canal than is good for it, damaging the canal in the process (of dilation, or sex). It may also be impossible to dilate enough to not lose depth (length) or width because at some point you no longer have time to spend 4 hours a day on dilation and the cleanup. It may become impossible to dilate if the canal has gotten so shallow or narrow that the dilators are all too big, this can also make it hard to douche to clean out the canal. The result may be that the canal ends up with a pocket at the end that collects mucous, lube, body fluids (from sexual intercourse) and if it is not possible to douche well, this might result in infections and discomfort.
Diverticulum
Small sacs or pockets that can form in the (neo)urethra (urethral diverticulum) that fill up with urine. This may be accompanied by pain, frequent urinary tract infections, incontinence, or blood in your urine. This needs to be corrected with surgery.
A female who underwent phalloplasty genital surgery experienced a lot of complications including urethral diverticulum in her urethra. The diverticulum keeps filling and got infected so needed to be drained requiring her to wear a catheter again (see Exulansic's video 'Phalloplasty Philes: Your Own Portable Lake Lanier').
Embolism
This is when an artery is blocked by a foreign body such as a blood clot or air bubble. One cause of this is when a blood clot from the deep veins in your leg (deep vein thrombosis, DVT) breaks off and travels to another part of the body where it blocks blood flow. A pulmonary embolism is a blood clot like this that gets stuck in your lung artery where it blocks blood flow to your lungs. This is an emergency. See https://www.nhs.uk/conditions/embolism/. One patient who had phalloplasty genital surgery experienced a host of complications including bilateral pulmonary embolism (blood clots in both her lungs, but also her legs and pelvic area, she also had a urinary tract infection that developed into a kidney infection, it was bad; see Exulansic's video 'Phalloplasty Philes: Requiem for a Peen (Gruffin)).
A female reddit user describes how she underwent phalloplasty genital surgery and ended up with bilateral (on both sides) pulmonary embolisms with the beginning signs of tissue damage, at only 24 years old. She had to stay in the hospital for three additional weeks and ended up with a relatively short phallus at 3" in length 'on a good day' but the urethra hole at the top healed over so she needs another surgery to fix that (see Exulansic's video 'Phalloplasty Philes: The No-Eyed Trouser Snake').
Erosion or fracture of erectile device/implant
Some people who have undergone phalloplasty choose to have an inflatable erectile device implanted in the neophallus to imitate an erection. These devices are developed for males with erectile dysfunction so naturally their use in a surgically-created ‘penis’ will be experimental: a neophallus does not have the same anatomy as a penis. However, a new erectile device is being developed currently (in 2023) specifically for the neophallus. With the devices developed for males it is possible for the implant to erode out of the phallus, meaning that parts of the implant put pressure on the tissues and skin to the extent they are ‘working their way out’. This will need to be corrected in a surgery to prevent the skin from being broken and the parts of the device sliding out through the open wound (with the risks of infection that come with an open wound). One reddit user who posts on the phallo subreddit has seemingly had over 25 procedures related to her phalloplasty including several replacements/fixes of her inflatable erectile device, and this was all when she was in her late teens to early/mid 20s. As of July 2023 her phallus has failed after about 5-6 years since the first surgery because of a lot of internal scarring due to use of the erectile device, so the device had to be permanently removed leaving a short, creased neophallus. She is now considering a complete redo of her phalloplasty to try again... It is also possible to instead of an inflatable erectile device choose the semi-rigid rod implant (also called malleable penile prosthesis). This is a pair of rods that are implanted into the 'shaft' of the phallus and are anchored to the pubic bone. The implant is bent upwards for sex and downwards to be 'flaccid'. The rods themselves can fracture, although this appears to be rare, see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4811081/.
Fistula
This is when an abnormal tunnel forms between two internal organs or an internal organ and the outside of the body. A fistula usually does not heal on its own and will usually require surgery to resolve. It is possible to have multiple fistulae at the same time. If one forms between your urethra (pee tube) and the outside of your body, you will leak urine from it when you pee. This is very common in women who choose phalloplasty with urethral lengthening. The result is that they will pee from one or multiple sites aside from the tip of their phallus, spraying urine everywhere. It is also possible for a fistula to form between the rectum or colon and the neovagina. The person may then leak faeces through the neovagina and/or get infections in the neovagina because poop bacteria are getting inside the canal. They wil also have problems with foul odour.
One story of a male who had a vaginoplasty who developed a fistula resulted in a temporary loop ileostomy causing him to become suicidal (see Exulansic's video 'Vaginoplasty Volumes: Tuck Everlasting (Reddit Chronicles)').
A female reddit user who underwent metoidioplasty genital surgery four weeks prior ended up with a fistula at the base of her 'scrotum' that leaks when she pees even if she tries pushing toilet paper onto it. Another user chimes in saying she experiences the same issue having developed a fistula after the initial surgery, but in her case she also had two failed repair surgeries so now 16 months after the initial surgery she is still dealing with a fistula (see Exulansic's video 'Metoidioplasty Moments: A Fistful of Fistula').
A female TikTok user who underwent phalloplasty genital surgery seemingly developed a fistula with urine coming out from around her 'scrotum' that required additional surgery to fix (see Exulansic's video 'Phalloplasty Philes: Pissing into the Windmill').
Another story is that of Ryan James, a female who had phalloplasty surgery. She developed a fistula and had to have a colostomy as a result of the vaginectomy (removal of the vagina) as part of the phalloplasty procedure (see Exulansic's interviews with Ryan James).
Granulation
Granulation tissue is a type of new connective tissue. This can form when healing from surgery. Pink granulation tissue is considered an indicator of healing. But unhealthy granulation tissue is dark red, often bleeds when touched, and may indicate the presence of wound infection. The latter may need to be treated. If it doesn't heal and causes other issues with the vaginoplasty, a repair surgery may be needed such as in the case of a male who had undergone rectosigmoid neovagina surgery but who had genital granulation tissue and also stenosis (narrowing) of the introitus (opening of the canal). The patient had two surgical revisions but this didn't help. The surgeons then used pig bladder tissue to try to fix the neovagina, see https://pubmed.ncbi.nlm.nih.gov/30413867/.
Haematoma
A form of localised bleeding, a bruise. This occures when veins or arteries are damaged (for instance, by a direct hit) and blood collects outside of the veins/arteries. This can result in a hard mass that changes colour over time as it heals. It is possible to develope a haematoma from surgery and when severe, the haematoma may require surgery to drain the blood that collected and/or control the bleeding. There is an infection risk associated with haematomas. See https://sanaramedtech.com/blog/treating-post-surgical-seroma-hematoma/.
A female who had metoidioplasty genital surgery developed a haematoma that kept refilling that needed to be squeezed/drained. Based on her own video it seems this was a very painful and traumatic experience (see Exulansic's video 'The Artery of War'; she also had an arterial bleed).
Hair growth inside neovagina/neourethra
During genital surgery the surgeons may use skin that grows hair to create the neovagina canal or the neourethra (such as base of the penis, the scrotum, the arm or leg or abdomen, or groin). Even when the patient underwent permanent hair removal of this skin before surgery, it is possible for some hairs to still come back and grow inside the neovaginal canal or the neourethra of the phallo. It is very difficult if not impossible to remove such hairs when the surgery has already been performed. It is possible for those hairs to grow as ingrown hairs and become infected, or for the hairs to cause infections even when not ingrown. There are stories of people being able to feel hairs inside the neovaginal canal, or for hairs to come out of the phallus. Sometimes hair may not have been removed permanently from the phalloplasty donor site resulting in hair growth on the phallus and a need to shave the phallus.
Implant rupture
It is possible for implants to get a tear and break open, such as breast implants or testicular implants. This will require surgery to correct by removing the implant. Testicular implant rupture is rare, but it is conceivable for this to be less rare when done in females if their 'scrotum' is positioned further down in between the thighs/with thicker thighs.
Incontinence (urine and/or faeces)
Incontinence is the inability to retain body fluids. Urinary incontinence is the unintentional passing of urine. Faecal incontinence, or bowel incontinence is when someone struggles to control their bowels. Both conditions can result from transgender genital surgeries due to these surgeries working with urogenital tissues and with/near the intestines. These conditions are often embarrassing and upsetting and can cause people to smell of urine or poop even if they frequently bathe. It may be difficult to deal with incontinence and sometimes surgery might be required. If you have run out of surgery options for urinary incontinence, you may need to use pads and pants or a catheter for life. For bowel incontinence there are pads to wear or a plug to insert in your rectum, drugs to change your stool, or surgery to fix damage or place an electronic device to help the anus work better (for sacral nerve stimulation) or injection of bulking agents to help make the anus stronger. Sometimes a colostomy is the best solution. There are several women who have undergone transgender genital surgery who ended up with a colostomy long-term and possibly permanently. There is a male patient who underwent vaginoplasty who ended up unable to empty his bladder and with an inability to pass stool which required such a sacral nerve stimulation implant (see Exulansic's video 'The Piss Toll').
Infection
The invasion and growth of germs (bacteria, viruses, yeast, fungi) in your body. Whenever your body is cut there is a risk of infection and although a lot of measures are taken during surgery to reduce the infection risk, it is possible to end up with an infection from surgery. It is possible to get sepsis from an infection.
In 2017 a research paper was published describing a case study of an 18-year-old trans-identifying male who underwent vaginoplasty surgery resulting in a severe E. coli infection that caused septic shock and multi-organ failure resulting in death, see https://www.sciencedirect.com/science/article/abs/pii/S1083318816301747.
There is a story of a female who underwent a phalloplasty genital surgery who experienced a lot of complications including numerous infections: urethral infection, staph infection, MRSA infection, septic shock, and Clostridium difficile infection. She may have had to undergo 10 surgeries as part of this effort to get a penis. She also had pulmonary embolisms and has hair growing on her phallus (see Exulansic's video 'Phalloplasty Philes: #1 Fan').
A female who underwent phalloplasty surgery developed an abscess on her arm at the site where surgeons placed a rod/tube under the skin hoping the surface of the rod would scar over so that this newly created 'tunnel' could later be used as the 'urethra' in the neophallus, see https://onlinelibrary.wiley.com/doi/full/10.1002/cia2.12137.
Infertility / sterility
Blocking puberty and/or using cross-sex hormones can affect someone's fertility whilst taking the drugs. It is not that clear whether this kind of drug use affects long-term fertility if someone were to stop taking these drugs. Time will tell. What is clear is that when the gonads (ovaries, testes) are removed, the person is permanently sterile. This means a male will not be able to father children, and a female will not be able to mother children. If a female has her uterus removed she will not be able to carry a pregnancy using another woman's egg either. Some trans-identifying people 'bank' sperm or eggs before they start using hormones in case they want to have their own child in the future. Some people stop their hormones for some months to start producing their own sperm/eggs to then 'bank' them, before continuing their hormone use. Creating a sperm sample is very simple as it requires maturbation into a collection cup if the male is able to do so. If this is not possible, the doctor can extract sperm directly from the testes but this is a medical procedure and thus more invasive than masturbation. Females will need to undergo hormone treatment to produce multiple eggs that are then collected using a needle that goes into the body. Embryos survive better than eggs when they are frozen so some females choose to have the collected eggs fertilised with someone's sperm (either their partner's or a sperm donor). This may mean that an underage female is using a sperm donor to fertilise her eggs so she has embryos for the future, meaning that the sperm donor's sperm is used to create embryos with eggs taken from a child. More experimental medical procedures include taking some ovarian tissue and keeping it in the freezer to try to use later to create eggs.
It is important to consider that there are no guarantees with fertility methods. Especially in the case were a female no longer has her uterus (but she does still have her ovaries or she has already banked eggs or embryos), her options to become a parent may be limited as gestational surrogacy (where another woman carries a baby that is not genetically related to her as she did not provide the egg) may be illegal in some countries or it may be illegal to pay a woman for this 'service' resulting in very few women wanting to be a surrogate (this also applies to gay male relationships where by definition there is no female). Even if commercial surrogacy is available, this may not be covered by insurance and the costs may be around $50k-100k (2023 estimate).
Loss of sensation
The loss of the ability to sense with a part of your body, for instance due to nerve damage from surgery. The affected area or body part may no longer be able to feel any touch or may not feel hot/cold or may not feel pressure anymore. This may only affect a small area or might affect a larger area. If this is only a small area on your leg, this may not be such a big deal. But a small area in your genital area may encompass most of your genital so the damage may have a much larger effect on your life. Loss of sensation in your hand may be dangerous if you can no longer feel hot/cold or pressure as you might end up hurting yourself without realising it.
Necrosis
Permanent death of tissues due to a lack of blood flow to this tissue. It is possible for parts of the neovagina or neovulva to become necrotic and fall off or requiring removal. It is also possible for this to happen to part or all of the neophallus (called ‘flap failure’ or ‘flap loss’). This can also happen to tissues in the area of the phalloplasty donor site if blood flow to it has been affected such as in a reddit user who had tissue in her leg (her donor site for phalloplasty) rot.
A case is described in which a male who received what was considered a successful recto-sigmoid vaginoplasty 18 months prior experienced a life-threatening small bowel obstruction. The authors warn that it is possible to get such a life-threatening complication at any point after the surgery: "The rate of adhesive small bowel obstruction is highest in the early period of any intra-abdominal post-operative surgeries, but the risk remains life-long. Transgender women receiving complicated vaginoplasty should be instructed to continue long-term follow-up to ensure early detection and management of post-operative complications." (see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6232285/). This suggests that after such a surgery the patient may at any point in the future need specialised urgent/emergency care. How would this knowledge affect someone's life? If patients are made aware of this risk, will they still go on backpacking holidays where they may be hours away from the nearest road? Will they be worried about any periods during which they may not have healthcare insurance and will they go into major debt if they need this surgery during such a period without insurance? Are patients even told about this life-long risk before they undergo this surgery?
Neovaginal prolapse
This is the term for when the neovaginal canal is not properly attached inside the hole in the pelvic area and partially or fully comes out of the opening in the perineum. This will require surgery to correct and may mean loss of the canal. A study published in 2014 reported that between 4-12% of males who had vaginoplasty experienced a partial or total prolapse dependent on the the technique used to attach the canal, see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4033431/.
Nerve damage
It is possible for nerves to be damage during surgery. This can result in changed sensation such as tingling, numbness, burning, loss of sensation, muscle weakness, or pain. This can resolve over time or be corrected with surgery, or may be permanent.
Pain
It is expected to experience pain after a procedure when you have maxed out your pain medication or are coming off of pain medication, and healing can hurt too. But this is expected to get better over time over a period of weeks and a couple of months. However, it is possible to keep experiencing pain or dyscomfort after surgery even months or years later.
Shape Shifter experienced intestinal cramps during sex in his colon vaginoplasty because, according to his knowledge, the colon used to create the neovaginal canal remains part of the digestive system, at least with regards to the nerves and how the brain interprets pain in that tissue. The colon is adapted to process (soft) stool as part of the digestive process, not to be touched from the inside with fingers, dilators, dildos, or a penis. He talks about his experiences undergoing several vaginoplasty surgeries and revisions on his YouTube channel.
A TikTok user who underwent metoidioplasty genital surgery still had a lot of pain 2.5 months after her surgery. Based on her video it is also clear she did not fully understand the surgical technique, underestimating how invasive the surgery was going to be and not being prepared for the amount of pain she was going to be in (see Exulansic's video 'Metoidioplasty Moments: Angry Camel Pose').
Patrick, one of the persons being interviewed as part of the 'Zembla' TV show on transgenderism, explains how years after his vaginoplasty he still experiences pain and dyscomfort in his pelvic area and bladder. He no longer identifies as a transwoman and instead now sees himself as a gay male. He no longer has male genitalia so he feels like his life is ruined by the medical interventions he underwent as part of his gender transition.
Pregnancy whilst on testosterone
Testosterone is a teratogen meaning that it can cause birth defects when a pregnant female uses the drug. In sheep, exposure to testosterone affected development of female foetuses (see https://academic.oup.com/endo/article/146/7/3185/2500473). In mice, testosterone affected development of the genitals in female foetuses (see https://www.pnas.org/doi/full/10.1073/pnas.1610471113).
There are suggestions that prenatal and neonatal testosterone exposure may affect human behaviour (see https://pubmed.ncbi.nlm.nih.gov/17084045/; for a study on monkeys, see https://www.sciencedirect.com/science/article/abs/pii/S0018506X09000658).
Replacement of erectile device/implant
Erectile implants are developed for males who have a penis but suffer from erectile dysfunction. These devices/implants are estimated to have a life expectancy of 5 to 20 years . This data will come from male patients, possibly older on average than the females who opt for phalloplasty with an erectile implant. It is also conceivable that male patients are less active with the implant if they are on average of older age than the females who get this, so it is conceivable that the implant will last less long as it is used more. Moreover, the neophallus is not a penis so possibly higher risks of erosion may limit the lifespan of the implant in females. If you get the implant at age 20 or 30 and you may need to get it replaced every 10 years, this means 3-5 more surgeries later in life, possibly a lot more if you wear out the device faster.
Revision surgery
If the initial surgery did not leave you with the aesthetics you wanted and/or there are functional issues with your surgery results, you may want/need a revision surgery. Another surgery means another general anaesthesia and another situation in which you are taking risks. Moreover, there is no guarantee that whatever the issue is that makes you choose/need a revision will be solved for good.
Sepsis
Septicaemia, blood poisoning. A life-threatening reaction to an infection resulting in damage to your tissues and organs. This needs treatment in the hospital immediately.
A male who underwent vaginoplasty surgery and then revision surgery for it, and some month later got larger breast implants (he already had implants before) was found grey, cold and unresponsive by his boyfriend. His implants were very infected causing a kidney infection and then sepsis and kidney failure causing him to 'nearly die'. He got a secondary infection in his chest too. If he had been found any later, he may very well have died (see Exulansic's videos 'Vaginoplasty Volumes: Through the Eye of the Needle' and 'Get well soon, Ruby Fiera!').
Seroma
A seroma is a sterile collection of fluid under the skin, usually at the surgery site. The body may do this to fill up space after tisse has been removed. When a seroma is large or causes pain, it may need to be drained by needle and syringe and a drain may be put in. It is possible for a seroma to come back and to need to get it drained multiple times. A seroma may become infected or turn into an abscess. See https://sanaramedtech.com/blog/treating-post-surgical-seroma-hematoma/.
Sexual dysfuction
Surgery to the genitals may affect sexual function. A study on males who had undergone robotic peritoneal flap vaginoplasty showed that of those who had this surgery at least one year before the study was conducted, 14% were not able to experience orgasm, this was not correlated with orgasmic ability before surgery but was negatively related to smoking history, see https://pubmed.ncbi.nlm.nih.gov/35337785/. A 2018 study that included males who had undergone penile inversion vaginoplasty found that 26% were unsatisfied or highly unsatisfied with neoclitoral sensitivity and that a 33% were unsatisfied or highly unsatisfied with neovaginal depth and 10% of patients did not experience orgasm, see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5994261/. A meta analysis (reviewing many studies who report on patient outcomes) showed that the ability to achieve orgasm was 76% in patients who had undergone vaginoplasty surgery meaning that 24% of those patients were not able to experience orgasm. This low average was mostly due to penile inversion vaginoplasty, the most common form of vaginoplasty, with 73% being able to have an orgasm. The patients who underwent a form of intestinal vaginoplasty had better results with 95% being able to achieve orgasm. The patients who underwent intestinal vaginoplasty had a higher proportion of fistula, stenosis and strictures, and prolapse than the males who underwent penile inversion (see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7984836/). From this study it is not clear whether the studies they included managed to follow up on all the patients on who they performed this surgery.
Then there's the story of Jazz Jennings who after puberty blockers and cross sex hormones had a botched vaginoplasty surgery (because he did not have enough genital skin to work with due to his puberty being blocked; he needed multiple revisions and the surgeons ended up taking skin grafts from his upper thigh area). Jazz seems to be struggling with sexual funtion. Trans-identifying male surgeon Marci Bowers was involved in some of Jazz' vaginoplasty surgeries and is reported as having stated that if a someone has never experienced orgasm before surgery and their puberty has been blocked, it is very difficult to achieve that afterwards. He acknowledges this is an overlooked problem and he wonders how this will affect the patient's long-term happiness if they are not able to be a responsive lover (see https://www.psychologytoday.com/gb/blog/women-who-stray/202111/does-affirmative-treatment-impair-sexual-response-in-trans-youth).
A story of a female reddit user who underwent metoidioplasty genital surgery describes how at four months after the surgery she is still struggling with sensations in her genital area. She can only feel half of her micro "penis" and the sensation she does have she describes as 'half pleasurable and half just uncomfortable' (see Exulansic's video 'Metoidioplasty Moments: The Piss Nick').
Oestrogen use by males is associated with a decreased libido and can cause erectile dysfunction. This can result in the penis shrinking. The testicles are also expected to shrink. Vaginoplasty may rely on the penile and scrotum skin to create a 'convincing' neovulva and neovagina so shrinking of this 'source' material may pose issues when the patient wants to undergo vaginoplasty.
Testosterone use by females can cause vaginal atrophy (thinning and drying of the vaginal tissue making it more fragile) and pain during sexual intercourse.
See the following paper for a discussion of affirmation-only treatment for transgenderism and the role of the placebo effect (including a discussion on sexual function): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9886596/.
Stenosis, stricture
A narrowing of a structure. It is possible to have stenosis in the neovagina canal making it painful and/or difficult or even impossible to dilate and have sexual intercourse. This can make it difficult to clean the inside (douching) which may result in unpleasant smell or infections.
Shape Shifter is a male who has medically transitioned but regrets his genital surgeries. He developed stenosis of the canal almost immediately after surgery. Three revision surgeries to help correct the stenosis resulted in him developing a colorectal fistula. This fistula was torn back open during his fourth revision surgery and no surgeon will help him now as they suspect that another revision surgery may leave Shape with a colostomy bag, see https://reduxx.info/opinion-the-boy-who-shifted-shapes/ (and see Exulansic's video 'Vaginoplasty Volumes: The WPATH of Least Dehiscence' and the videos in which Exulansic and Shape Shifter interview each other).
Another male who underwent vaginoplasty experienced vaginal stenosis, requiring the canal to be replaced in an additional surgery, 8 months after the initial surgery (see Exulansic's video 'Update on Rumer Has a Clit Dude').
It is also possible for a (neo)urethra made as part of a metoidioplasty or phalloplasty to become too narrow. This restricts the flow of urine and may cause diverticuli and infections such as urinary tract infection. Stenosis or stricture may make it impossible to fully empty the bladder which might make the patient not drink enough water because they have such difficulty passing urine, which can in turn cause kidney stones or bladder stones. This also increases the chances of getting a urinary tract infection (UTI).
Stroke
An ischaemic stroke is what occurs when the blood flow to part of the brain is cut off. This can be due to a blood clot or air bubble (embolism) blocking the flow of blood. A hemorrhagic stroke is when an artery in the brain ruptures or leaks putting pressure on the brain which damages the brain cells. A mini-stroke (a transient ischemic attack) blocks blood flow only for a short time (less than 5 minutes). It is possible for a stroke to be a surgical complication.
A 30-year old male experienced a stroke during facial feminisation surgery. His complaints were ignored by hospital staff and when he eventually did get appropriate medical care elsewhere (emergency services), he had lost the ability to use one of his arms, from which he never recovered so he now has a permanent disability. It turns out that during his facial feminisation surgery they severely damaged his carotid artery and that as a result he had suffered a stroke in his right frontal lobe resulting in brain damage (see his reddit post titled 'I thought FFS would change my life, but not like this... (Dr. Alex Kim)' and Exulansic's video 'Facial Feminization Fumbles: A Sense of Humerus').
Suicidality
Despite activists claiming that gender transition is the only way to prevent transgender people from wanting to exit this world, there are people who after medical transition remain/become suicidal. Patrick, a Dutch man, is one of these people. He is interviewed in the 'Zembla' documentary on transgenderism in which he shares his lifelong struggles with severe mental health issues and substance abuse. He was failed by the medical system who on his first attempt to get help for transgenderism recognised he was not transgender, but when he tried again at another clinic some years later he, in his experience, was affirmed and encouraged to medically transition. He underwent vaginoplasty surgery that he now deeply regrets. He now no longer identifies as a transwoman but as a homosexual man. He no longer has male genitalia and he experiences dyscomfort in his pelvic area and his bladder and he is struggling with severe mental health issues to the point where he is contemplating assisted suicide, for which he has been approved (in the Netherlands, assisted suicide is allowed in certain circumstances).
Some scientific data suggests gender-affirming treatment may reduce suicide-related outcomes (see https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10027312/ for a narrative review), but some of these studies suffer from issues such as no data on suicidality before treatment, not controlling for other mental health issues, or loss to follow up (not being able to contact every person that underwent gender-affirming treatment in your clinic; it is possible that the proportion of people with regret, a bad outcome, or the worst outcome: suicide, is higher in those patients the clinic is unable to contact). These studies usually only look at people who received affirmation treatment (drugs and surgeries) and do not compare the outcomes for this group to a group with the same diagnosis who get no treatment or who get another kind of treatment (such as talk therapy or any other kind of therapy/treatment for mental health). It is then not possible to say which kind of treatment is superior when it comes to reducing suicidality (or compare any other kind of outcome).
Testosterone gel transfer
One method for taking the drug testosterone is by a gel that is applied onto the skin. The testosterone will be absorbed from the gel into the skin. One practical problem with this is that it is possible for others around the patient to be exposed to this testosterone by touching the patient's skin where the gel was applied or possibly through sharing a towel or bedding on which the gel is rubbed off. This testosterone exposure can be harmful to children of both sexes and to women. A case in the literature describes a 31 year old woman who had grown more body hair in the past year. Her testosterone level was measured as being 6.7 nmol/l at the highest when less than 2.5 nmol/l is considered normal. Her partner used testosterone gel for a medical condition but he was not aware of the recommendation to take a shower or cover the area where he applied the gel before having physical contact with others. When he stopped using the gel, her testosterone level went back to normal. When he started using the gel again, despite explicit instructions to cover the application site or shower before contact, the woman's testosterone level increased again. The male then switched to injecting testosterone and the woman's testosterone went back to normal (see https://academic.oup.com/humrep/article/24/2/425/808493). This illustrates that apparently instructions were not given or followed, and that even after the partner was exposed to testosterone and explicit instructions to reduce transfer, the female partner was still exposed to testosterone.
A publication describes two cases of transfer of testosterone gel from fathers (males using this gel for medical reasons) to their children. The first case involves a two year old boy whose penis had grown, who was experiencing frequent erections, who was growing pubic hair, and who had grown taller in the past few months. The penis was at Tanner class (stage) III which is usually seen in boys around age 13. He had a very high level of testosterone for his age and his bone age had advanced by three years. The changes seemingly reversed once he was no longer exposed to testosterone gel. The second case involved a 6 year old boy who had started growing pubic hair and growth of the penis in the past few months. He was also tall and had advanced bone age. His exposure was suppressed but he nevertheless started puberty. Read about both cases here: https://www.elsevier.es/en-revista-endocrinologia-diabetes-nutricion-english-ed--413-articulo-potential-consequences-in-children-testosterone-S2530018017300768.
The UK government includes information on this topic on its website stating a risk of harm to children following accidental exposure to Testogel (a testosterone gel). They warn of premature puberty and genital enlargement in children who were in close physical contact with an adult using testosterone gel and who were repeatedly exposed (see https://www.gov.uk/drug-safety-update/topical-testosterone-testogel-risk-of-harm-to-children-following-accidental-exposure).
Urination / voiding issues
It is possible to severely damage the ability to urinate with gender genital surgeries. There is the story of a male who got vaginoplasty surgery and now has to use the bathroom to pee every one or two hours including when he wants to sleep (see Exulansic's video 'Jacob's Bladder'). There are also the stories of many females who had gender genital surgery who ended up with urination difficulties such as Gruffin (covered extensively by Exulansic) who developed bladder stones (in addition to nearly losing a leg and nearly dying from blood clots). Many females who get phalloplasty appear to struggle to complete urination and after peeing always have some urine dribble out of the phallus no matter how much they squeeze and push and jump and wiggle.
UTI
UTI stands for urinary tract infection. It encompasses infections of any part of the urinary system: the kidneys, ureters, bladder, and urethra. If someone struggles to urinate or can not fully void their bladder they might be at a higher risk of developing a UTI. This may start in the urethra and if not successfully treated can develop into a bladder infection or even a kidney infection.
Vocal damage
It is possible for males who get so-called vocal feminisation surgery to end up with damage to their voice losing part of their vocal range and for their voice to seemingly stop working as described by one such patient posting on reddit (see Exulansic's video 'Tracheal Troubles: Falsetto Hope').
Wound dehiscence / wound separation
This is the term for when a surgery incision reopens. This can be the result of an infection, pressure on the sutures, poor suture technique, or decreased blood flow. This may require medical attention to resolve. This is seen in some people who undergo gender genital surgeries and wound separation can increase the risk for infection, can cause more scarring, and can change what the end result looks like.
One such example of a patient with wound separation is Rylan who chose to undergo a cosmetic double mastectomy for gender reasons. Because of her obesity she had few surgeons to choose from (surgery is more risky on obese people so most surgeons will have a BMI cap for (cosmetic) surgeries). The surgeon that removed her healthy breasts neglected her concerns about issues with healing and wound separation despite frequent communication from Rylan to the surgical team. Rylan had to find emergency medical care elsewhere when she had a golfball-sized blood clot fall out of her wound whilst out in public. By this time she had been bleeding from the wounds for days. She then had to undergo another surgery to have over half a foot of flesh that had become infected with a bacterial infection removed. One of her nurses told her she could have gone septic had she not gotten this 'repair' surgery. You can read all about the surgeon who removed Rylan's healthy breasts here: https://lilymaynard.com/wielding-the-sidhbh-gallagher/, and view video content about this case in Ella Androphobia's video titled 'Dr. Sidhbh Gallagher - Necrotizing Gaslighter'.